Ultimate Guide to Rectal Prolapse in Broward County, Florida

Accepting all New Patients (Insured, Uninsured, Self Pay). Instant Appointments.




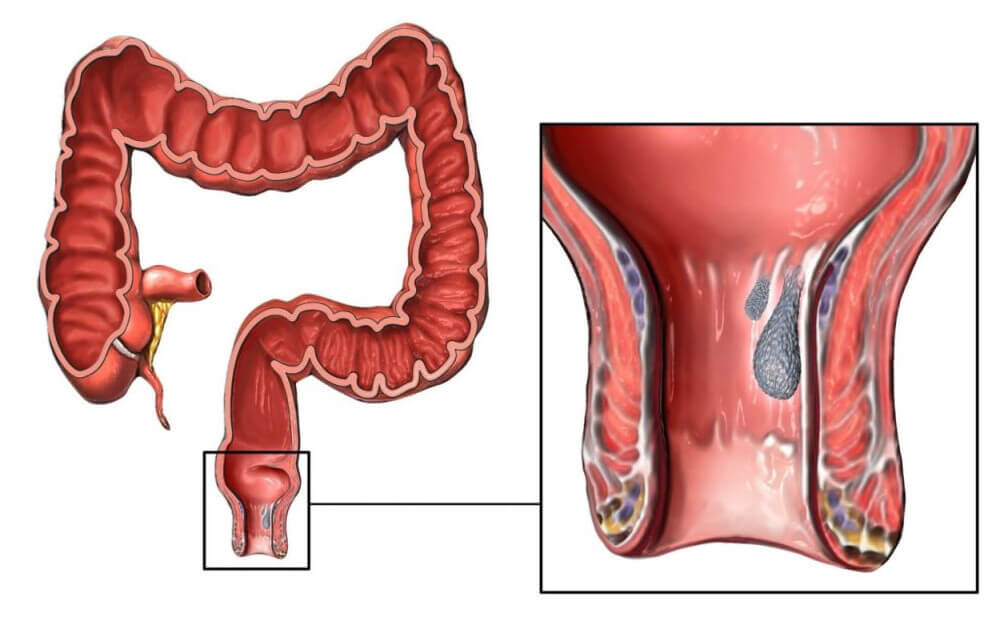
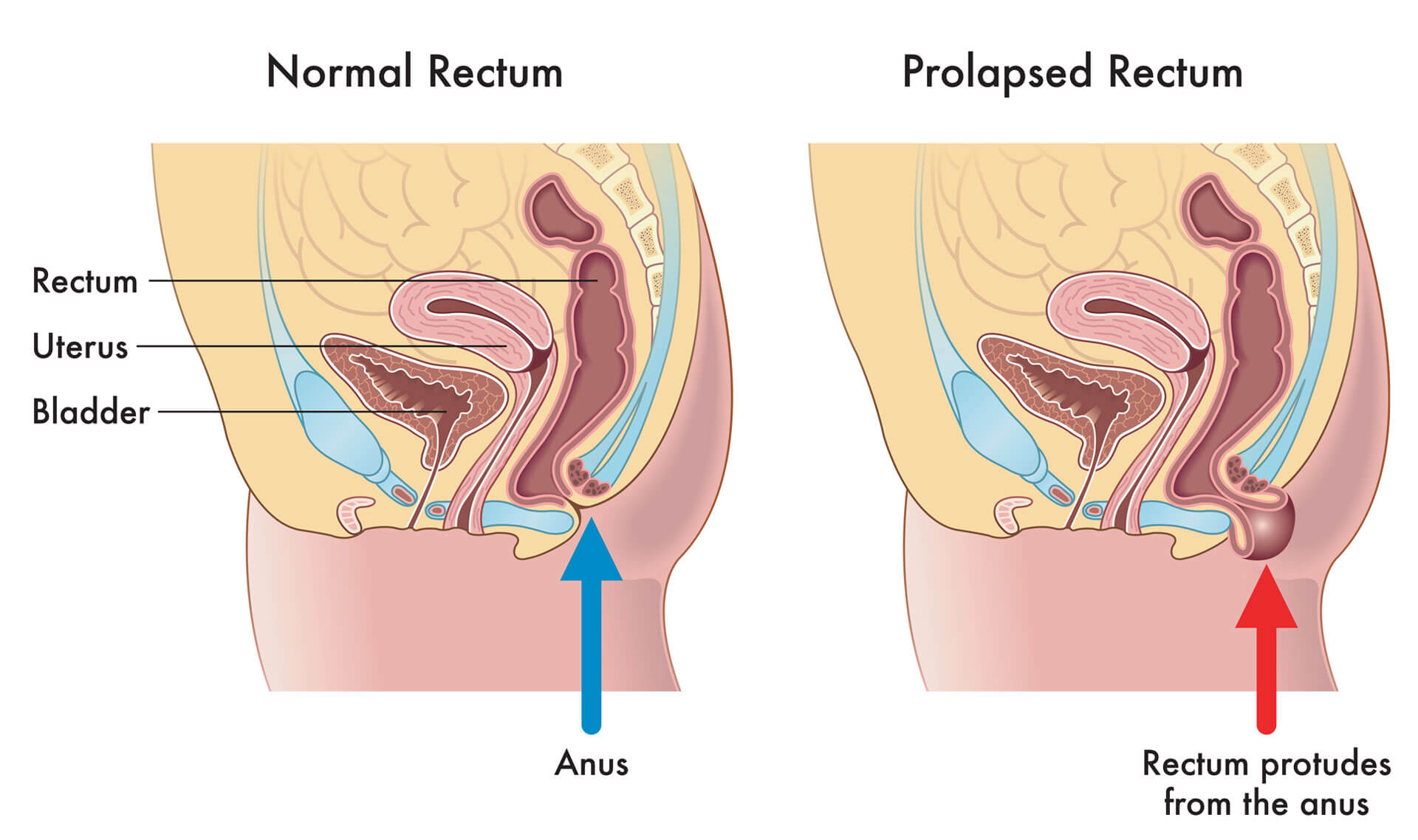
Rectal prolapse is a distressing medical condition characterized by the abnormal protrusion of the rectum through the anal opening. This condition results from the weakening or damaging of the supportive structures that generally hold the rectum in place within the pelvis. TThe final segment of the large intestine, plays a important role in eliminating waste from the body. When its integrity is compromised, it can lead to various symptoms and complications that significantly affect a person’s quality of life.
The primary types of rectal prolapse include partial prolapse, also known as mucosal prolapse, and complete prolapse, also referred to as full-thickness prolapse. In partial prolapse, only the inner lining of the rectum, known as the mucosa, protrudes through the anus. It typically appears as a reddish-colored mass during bowel movements and may retract back into the rectum afterward. Conversely, complete prolapse involves the entire thickness of the rectal wall protruding through the anus, forming a larger mass that may remain outside the body even between bowel movements.
Rectal prolapse is a medical condition that occurs when the rectum, which is the last part of the large intestine, becomes displaced and protrudes outside the body through the anus. This condition can be uncomfortable, embarrassing, and may require medical intervention to alleviate symptoms and prevent complications. Rectal prolapse can affect people of all ages, but it is more common in women over the age of 50 and in individuals with a history of conditions such as chronic constipation, pelvic floor dysfunction, or previous rectal surgery.
There are several factors are believed to contribute to Rectal prolapse development. Rectal prolapse is more common in older adults, particularly women who have given birth multiple times, but it can affect people of any age. Dr. Bhatt is reputed Colon and Rectal Surgeon for known for providing the BEST treatment for Rectal prolapse in Fort Lauderdale, FL, Pompano Beach, FL, Deerfield Beach, FL, Wilton Manor, FL, Oakland Park, FL, Davie, FL, Plantation, FL, Coral Springs, FL, Margate, FL, Coconut Creek, FL and Broward County, Florida.
Dr. Bhatt delve into the various facets of rectal prolapse, including its causes, symptoms, and the diagnostic procedures used to confirm its presence. Moreover, we aim to present a comprehensive overview of the available treatment options, ranging from non-surgical approaches to surgery, to effectively manage or completely resolve this condition. Additionally, we will explore strategies for prevention and long-term management, empowering individuals with the knowledge to minimize the risk of rectal prolapse and maintain a high quality of life.

Accepting all New Patients (Insured, Uninsured, Self Pay). Instant Appointments
Trustindex verifies that the original source of the review is Google. Dr. Astha Bhatt is an amazing colorectal surgeon who provides excellent care for hemorrhoids and diverticulitis. She explains every treatment option clearly, whether it’s office-based procedures like rubber band ligation or surgical options when needed. Her compassionate approach makes patients feel comfortable and supported, while her expertise ensures the best outcomes. Highly recommend her to anyone in Broward County seeking top colorectal care.Posted onTrustindex verifies that the original source of the review is Google. I had an excellent experience with Dr. Astha Bhatt, colorectal surgeon in Broward County. From the moment I met her, she made me feel comfortable and cared for. Dr. Bhatt is not only highly skilled but also very compassionate—she took the time to answer all of my questions thoroughly and treated both me and my husband with genuine kindness and respect. She explained my diagnosis and treatment options in detail and made sure I fully understood everything before moving forward. Her expertise in advanced robotic and laparoscopic minimally invasive procedures is truly impressive. With over 1,000 successful surgeries, it’s clear she is one of the best colon and rectal surgeons in Broward County, Florida. I would confidently recommend Dr. Astha Bhatt to my family, friends, and anyone seeking a caring, board-certified general and colorectal surgeon. She is professional, knowledgeable, and truly dedicated to her patients’ well-being. I would suggest him to my family members. One of Broward County, Florida's top colon and rectal surgeons.Posted onTrustindex verifies that the original source of the review is Google. Besides being a knowledgeable and skilled surgeon Dr Bhatt is also a caring person .I felt immediately comfortable as she addressed my questions and concerns and was quick to feel a high level of confidence that I was getting the best care possible. This the way healthcare should be..Posted onTrustindex verifies that the original source of the review is Google. There is little to no wait time. The staff were super polite and welcoming. The doctor was very helpful in addressing my needs.Posted onTrustindex verifies that the original source of the review is Google. As a diverticulitis specialist, Dr. Bhatt is a superb diverticulitis surgeon who shows considerable concern for her patients. Superb recuperation; she genuinely cares about her patients. She took the time to hear my worries and provided clear, understandable explanations of everything. They were obviously focused on figuring out the best option for me, and I never felt hurried. The entire transaction was seamless and comfortable thanks to the helpful and kind office staff. Without a doubt, I would suggest Dr. Bhatt to anyone searching for a skilled and sympathetic physician.Posted onTrustindex verifies that the original source of the review is Google. I have read everything about your work .it's sounds excellent..I see you soon. Thank you so muchPosted onTrustindex verifies that the original source of the review is Google. The top colorectal surgeon and proctologist for colon cancer treatment. Colon cancer can be cured if you have Dr. Bhatt on your side! Even though she is AMAZING, TOP quality, and even beyond top, what truly sticks out is how friendly she is. Dr. Bhatt listens carefully and is very clear about her objective of giving her patients the finest care possible and attaining the greatest possible result. She operated on my colon cancer, and I would suggest her as a surgeon to everyone I've spoken to. Dr. Bhatt would be my first choice if I ever needed a colon and rectal surgeon. She handles colorectal cancer and is an accomplished surgeon. The best care was provided. Patients are genuinely cared for by Dr. Bhatt. She is a skilled surgeon who treats colorectal cancer. The greatest care was given.
Recognizing the symptoms of rectal prolapse is crucial for timely diagnosis and treatment. Symptoms can vary depending on the severity and type of prolapse but commonly include:
Dr Astha Bhatt, Colorectal Surgeon, recommends diagnosis for people with Rectal prolapse upon having symptoms Rectal Prolapse.
It is important to follow these instructions closely and attend any follow-up appointments to monitor your progress. With proper care and adherence to the recommended guidelines, most individuals can expect to make a full recovery and resume their normal activities.
Detecting rectal prolapse typically involves a combination of medical history, physical examination, and diagnostic tests. Here’s how rectal prolapse is detected:
Medical History: Your healthcare provider will begin by asking about your symptoms, including any changes in bowel habits, pain, discomfort, or protrusion from the anus. They may also inquire about your medical history, including any previous surgeries, chronic health conditions, or factors that may contribute to rectal prolapse, such as chronic constipation or childbirth.
Physical Examination: During a physical examination, your healthcare provider will visually inspect the anus and rectal area. They may ask you to strain as if having a bowel movement to observe any protrusion of the rectum. They may also gently palpate (feel) the area to assess for any abnormalities, such as a protruding rectal mass.
Digital Rectal Examination (DRE): A digital rectal examination involves inserting a lubricated, gloved finger into the rectum to assess the tone, strength, and position of the rectal muscles and to feel for any abnormalities, such as a prolapsed rectum.
Proctosigmoidoscopy or Colonoscopy: These procedures involve using a flexible, lighted tube with a camera (sigmoidoscope or colonoscope) to visually inspect the rectum and lower colon. It can help confirm the diagnosis of rectal prolapse and evaluate for any other underlying conditions, such as inflammatory bowel disease or colorectal cancer or anorectal manometry, bad blood vessels, rectal prolapse occures fecal incontinence,.
Imaging Studies: In some cases, imaging studies such as magnetic resonance imaging (MRI) or defecography may be performed to provide detailed images of the rectal anatomy. These tests can help assess the extent of the prolapse and identify any associated abnormalities.
Defecography: This test involves the use of a dye in conjunction with imaging studies like X-ray or MRI. It helps to show structural changes in the lower digestive tract and assesses how the rectal muscles are working 20.
Fluoroscopic Defecography (FD) and Dynamic Magnetic Resonance Defecography (DMRD): FD has a higher detection rate for various anomalies and allows imaging in a more natural position. DMRD evaluates concomitant disorders, recal prolapse rectal prolapse, risk factors, part of the rectum and provides clear visualisation of pelvic anatomy, which is crucial for patients with previous pelvic or perineal surgery 22.
Anal Manometry and Endoanal Ultrasonography: These tests provide valuable information about anal sphincter function and allow precise imaging of the sphincter complex, respectively. They are essential for diagnosing fecal incontinence and identifying occult anal sphincter defects.
If rectal prolapse is suspected based on the findings of the examination and diagnostic tests, your healthcare provider will discuss treatment options with you based on the severity of the prolapse, your overall health, and your preference
Non-Surgical Interventions: Non-surgical treatments play a vital role in managing rectal prolapse, especially for patients who are not ideal candidates for surgery due to age or health conditions. Biofeedback therapy is a notable non-surgical intervention available at leading clinics. This physical therapy, conducted by specially trained physiotherapists, focuses on teaching exercises to strengthen the anal muscles. Patients learn to enhance muscles, recognize the urge for stool passage, and control it if untimely, potentially making surgery more successful by preventing recurrent rectal prolapse.

Accepting all New Patients (Insured, Uninsured, Self Pay). Instant Appointments.
What is the Optimal Treatment for Rectal Prolapse?
How Can I Prevent Rectal Prolapse from Worsening?
Are There Non-Surgical Treatments for Rectal Prolapse?
What Interventions Exist for Rectal Prolapse?

Accepting all New Patients (Insured, Uninsured, Self Pay). Instant Appointments.
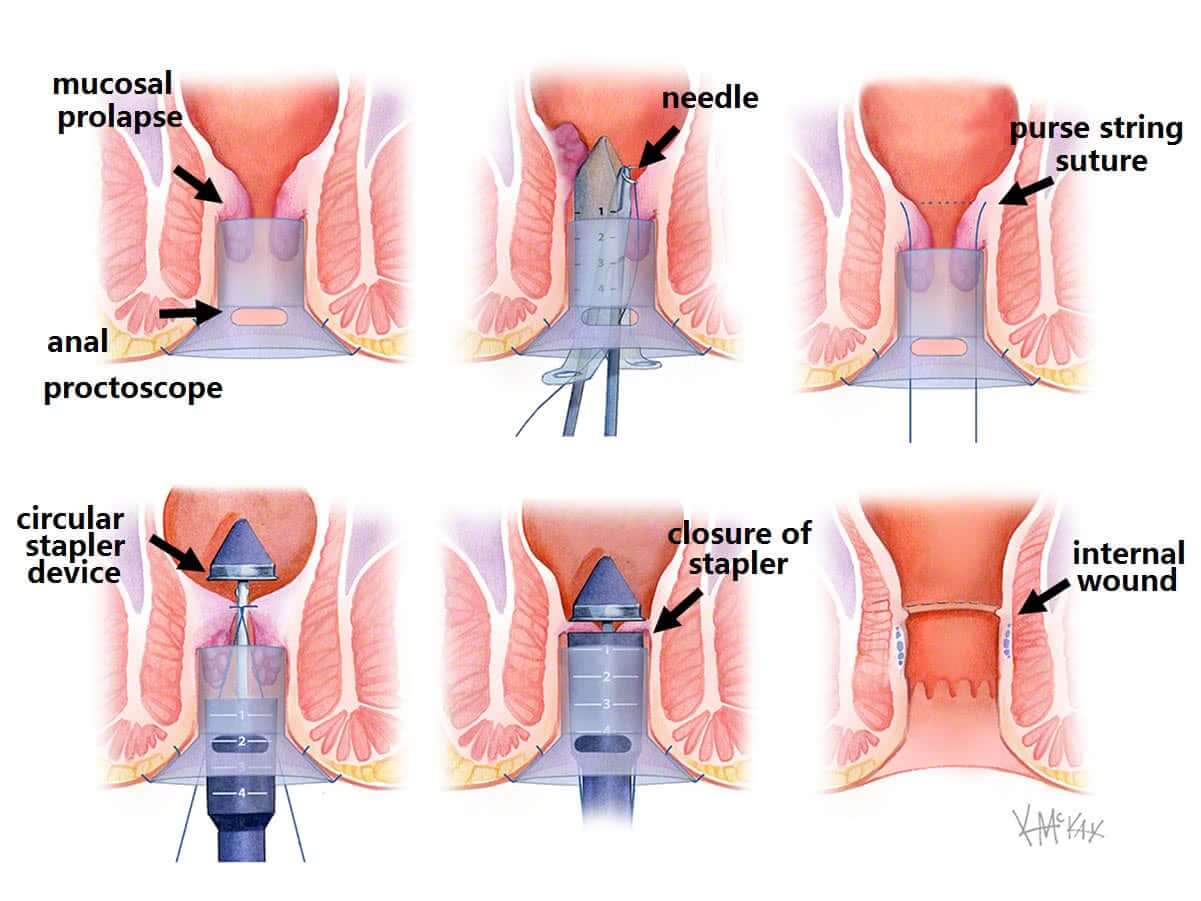
The long-term management of rectal prolapse primarily involves surgical intervention to correct the condition. Surgery, whether performed through the abdomen or via the anus, is aimed at tethering the rectum into place to prevent recurrence. Abdominal rectal prolapse surgery has been shown to provide better long-term results compared to perineal surgeries, with less than 5% of individuals experiencing a recurrence after abdominal rectopexy. In contrast, up to 1 in 4 people may face another prolapse after perineal rectopexy.
Postoperative care is essential for a successful recovery. Patients are encouraged to start ambulating and resume a regular diet from the first postoperative day, with most being discharged within 2 to 3 days. Despite the effectiveness of surgical treatments, some individuals may continue to experience symptoms such as constipation or the inability to completely empty the bowels. Additionally, women with rectocele may experience a recurrence of the problem in about 10% of cases
It is important to note that Dr. Astha Bhatt is recognized as a leading surgeon in the field of rectal prolapse, providing expert care and guidance in choosing the most appropriate surgical option for each patient. Her expertise significantly contributes to the positive long-term outcomes observed in patients undergoing surgery for rectal prolapse.
In conclusion, the prevention and long-term management of rectal prolapse involve a combination of lifestyle modifications and surgical interventions. Adhering to these strategies can significantly improve the quality of life for individuals affected by this condition.
A comprehensive exploration of rectal prolapse, from its underlying causes and symptoms to the meticulous details of diagnostic procedures, treatments, and critical preventative measures, we’ve underscored the multifaceted approach required to manage and overcome this condition. The significance of surgical intervention, particularly for those grappling with severe forms of prolapse, cannot be overstated. It is here that the expertise of Dr. Astha Bhatt, a forefront surgeon in rectal prolapse in Fort Lauderdale, FL, Pompano Beach, FL, Deerfield Beach, FL, Wilton Manor, FL, Oakland Park, FL, Davie, FL, Plantation, FL, Coral Springs, FL, Margate, FL, Coconut Creek, FL and surrounding area of Broward County, Florida comes into play, providing patients with tailored surgical options aimed at restoring quality of life and minimizing the possibility of recurrence.
As we conclude, it is imperative for individuals experiencing symptoms or those diagnosed with rectal prolapse to seek specialized care. We encourage you to schedule an appointment with expert Dr. Astha Bhatt, Colorectal Surgeon in Fort Lauderdale, Florida, to embark on a path toward recovery with the best in the field. The journey to healing begins with understanding the condition, weighing the treatment options carefully, and engaging with healthcare providers who are committed to offering not just treatment but a chance at an improved, prolapse-free life.
We encourage you to schedule an appointment with expert Dr. Astha Bhatt, Colorectal Surgeon who specialize in treating Rectal Prolapse in Fort Lauderdale, FL, Pompano Beach, FL, Deerfield Beach, FL, Wilton Manor, FL, Oakland Park, FL, Davie, FL, Plantation, FL, Coral Springs, FL, Margate, FL, Coconut Creek, FL and surrounding area of Broward County, Florida to embark on a path toward recovery with the best in the field. The journey to healing begins with understanding the condition, weighing the treatment options carefully, and engaging with healthcare providers who are committed to offering not just treatment but a chance at an improved, prolapse-free life.
Dr. Bhatt is experienced specialists who can accurately diagnose and effectively treat Rectal Prolapse using both non-surgical and surgical approaches.
Our mission is to provide personalized excellent care, guidance and service to all patients using the most advanced innovative technologies that are evidence-based.