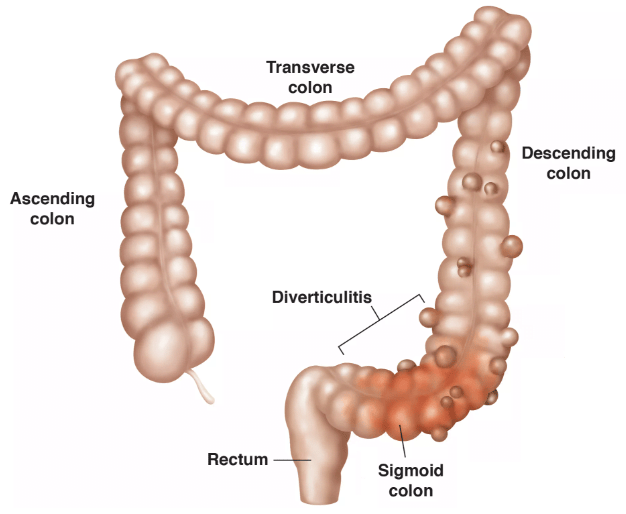
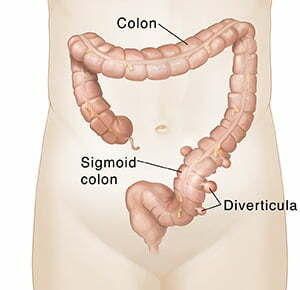
Sigmoid Colon Diverticulitis develops when the diverticula, which are small pouches that line the wall of the sigmoid colon, become infected or inflamed. This problem manifests itself through a variety of unpleasant symptoms, including obvious stomach pain, bloating, fevers, and an inconsistent bowel movement pattern, which paint a picture of your lower digestive tract in distress. This region, located in the S-shaped section at the lower end of your large intestine, is particularly vulnerable to such problems due to morphological and functional differences. Diverticula are very common, but when they get inflamed, that’s when diverticulitis turns from a silent spectator sport to an active participant one. This process highlights the need for medical intervention and highlights the delicate equilibrium found in our gut ecosystems. It also raises questions about the wider effects of lifestyle and dietary choices on our general health.
Diverticulitis is a disorder in which the digestive tract’s tiny, bulging pouches (diverticula) become inflamed or infected. These pouches usually occur in weak sections of the colon wall. Diverticulitis symptoms include abdominal pain (typically on the left side), fever, nausea, vomiting, changes in bowel habits, and, in some cases, rectal bleeding. It is frequently linked to a diet low in fiber and high in processed foods. Severe cases may necessitate medical intervention, such as antibiotics, pain medications, and, in some situations, surgery to remove the afflicted section of the colon.
The sigmoid colon Diverticulitis develops when the sigmoid colon’s tiny pouches (diverticula) become inflamed or infected. The sigmoid colon is the bottom section of the large intestine, right before the rectum. Diverticulitis normally develops when these pouches get clogged with debris, germs, or feces, resulting in irritation and, in rare cases, infection.
Diverticulosis and diverticulitis are two stages on the colon health continuum that are frequently mistaken yet have separate characteristics. Diverticulosis is a disorder in which small, benign pouches, or diverticula, are present along the colon wall. For many people, this problem lives silently, without causing any discomfort or demanding medical attention. It’s like having unnoticed guests who don’t disturb the household’s calm. Diverticulitis, on the other hand, develops when these innocuous visitors become a nuisance, resulting in inflammation or infection of the diverticulum. This transition from calm to chaos is marked by a number of indicators that necessitate attention and management. The transition from diverticulosis to diverticulitis is an important stage in patient care, necessitating a sophisticated knowledge and treatment strategy. Recognizing this distinction is critical in navigating the route to appropriate care and relief from Diverticulitis-related symptoms.
Taking the first steps toward controlling diverticulitis frequently requires a judicious combination of food changes and medication help. A fiber-rich diet is essential for this journey, allowing for smoother bowel movements and relieving strain on the colon’s walls, potentially preventing the beginning of future episodes. Antibiotics appear as a critical next step for patients dealing with illness, aimed at reducing inflammation and combating bacterial incursion. For those experiencing acute stages, switching to a liquid diet or introducing a period of bowel rest may be recommended, giving the digestive tract a much-needed break to promote healing. Engaging in this dual approach of dietary modification and medication underlines the proactive steps in addressing the symptoms and underlying causes of diverticulitis, setting the stage for a tailored treatment plan that resonates with the nuances of each patient’s condition.
Surgical intervention for Diverticulitis, particularly of the sigmoid colon, becomes a conversation when conservative measures—dietary changes and medications—prove insufficient. It’s a pathway considered for those grappling with complications that risk the integrity of the colon, such as recurring inflammation, the formation of abscesses, or the emergence of fistulas. In instances where the disease lays siege to the body with relentless episodes or leads to significant structural concerns, removing the affected segment through a sigmoid colectomy may be the most viable strategy to restore health and stave off further distress. This step is deliberated in depth with healthcare professionals, weighing the potential for a substantial improvement in quality of life against the inherent risks surgery carries. This decisive move towards surgery underscores the severity of a patient’s condition and marks a pivotal point in their journey towards recovery, tailored to those for whom other treatments have fallen short.
Diverticulitis, a condition marked by the inflammation or infection of small pouches in the colon, presents a complex challenge in the realm of gastrointestinal health. It beckons a nuanced understanding that, although a definitive cure remains elusive, effective management strategies offer a beacon of hope. Embracing a multifaceted approach that marries dietary vigilance with regular physical activity forms the bedrock of staving off acute episodes and promoting long-term well-being. The emphasis on a fiber-rich diet underscores the pivotal role of nutrition in softening the impact on the colon, thereby reducing the likelihood of flare-ups. Regular engagement in physical activity complements dietary efforts, aiding in maintaining a balanced body weight and fostering optimal digestive function. The journey with diverticulitis is one of proactive adaptation and management, where the power lies in the hands of the individual and their commitment to a lifestyle aligned with intestinal health. Engaging closely with healthcare professionals to tailor a management plan that reflects personal health goals and challenges is essential, illuminating the path toward minimizing the impact of this condition on daily life.
Embarking on the recovery journey post-sigmoid Colon Diverticulitis surgery, it’s crucial to adhere to a prescribed post-operative regimen. This encompasses a meticulous approach to medication adherence, a phased reintroduction of solid foods, and steering clear of vigorous physical exertion during the initial healing phase. Adjusting to post-surgery life may present its set of challenges, including managing discomfort and adapting to new bowel habits. However, these are typically transient states that improve with time. Proactive participation in follow-up care is key—ensuring open communication with your healthcare team to effectively monitor your healing trajectory. With diligent post-surgery care, individuals can anticipate a return to their daily routines, empowered by an enhanced quality of life.
You’ll be in the hospital for two to seven days following this procedure while your physicians watch you and ensure you can pass waste again.
When you get home, do the following to help you recover:
Dr. Astha Bhatt is a board-certified general surgeon with fellowship training in robotic colorectal surgerywith a focus on Best care for Sigmoid Colon Diverticulitis. Dr. Bhatt is the top colonoscopy surgeon in Broward County, including Fort Lauderdale, FL, Pompano Beach, FL, Deerfield Beach, FL, Wilton Manor, FL, Oakland Park, FL, Davie, FL, Plantation, FL, Coral Springs, FL, Margate, FL, Coconut Creek, FL, and neighboring areas.
Dr. Bhatt’s objective is to deliver customized quality treatment and service to all patients while utilizing the most sophisticated revolutionary evidence-based technology.
Dr. Astha Bhatt, MD
Dr Bhatt is a Board Certified General and Colorectal Surgeon, Proctologist based in Fort Lauderdale, FL, Pompano Beach, FL, Deerfield Beach, FL, Wilton Manor, FL, Oakland Park, FL, Davie, FL, Plantation, FL, Coral Springs, FL, Margate, FL, Coconut Creek, FL and surrounding area of Broward County, Florida. Dr. Bhatt provides one of the best comprehensive diagnostic treatments and surgery covering all aspects of Colon Rectal and General Surgery.
© 2024 Colorectal MD LLC. All rights reserved.